

We at NAS, are always committed to provide the highest level of member satisfaction and best
customer service experience. If you have any concern regarding your health insurance services,
please call our 24/7 customer care helpline and our team will assist and clarify your concerns. If
you feel this requires further escalation and investigation, please feel free to raise an official
complaint.
If you would like to raise a complaint, you may do so through any of the following channels:
Telephone: 800-2311 (Toll Free 24-7 Call Center)
Email: complaints@nas.ae
MyNas Mobile App: You will be required to register first before being able to log your complaint.
NAS’s Website: https://www.nas.ae/complaints/
Address: NAS Administration Services LLC, 4th Floor, Lulu Centre Building, Salama Street, Abu Dhabi, United Arab Emirates.
Please take note the following definitions (provided by the Dubai Health Authority) before
submitting your complaint:
Any expression of dissatisfaction by a customer, potential customer or other business partner or any regulatory body made to the company either directly or indirectly which is related to a product or service provided by the company or which is related to an employee of the company or which is related to a service provided by an intermediary acting on behalf of the company or provided by another business partner of the company such as but not limited to a health claims management company, hospital, clinic or physician.
Any expression of dissatisfaction concerning denial of coverage for a consultation, treatment or procedure which is clearly not covered under the policy or where the cost of the treatment exceeds the monetary limits under the terms of the policy are not complaints. However, where the cause of the complaint relates wholly or in part to vague wording or unclear definitions in the policy wording, terms and conditions or table of benefits this will be considered a complaint.
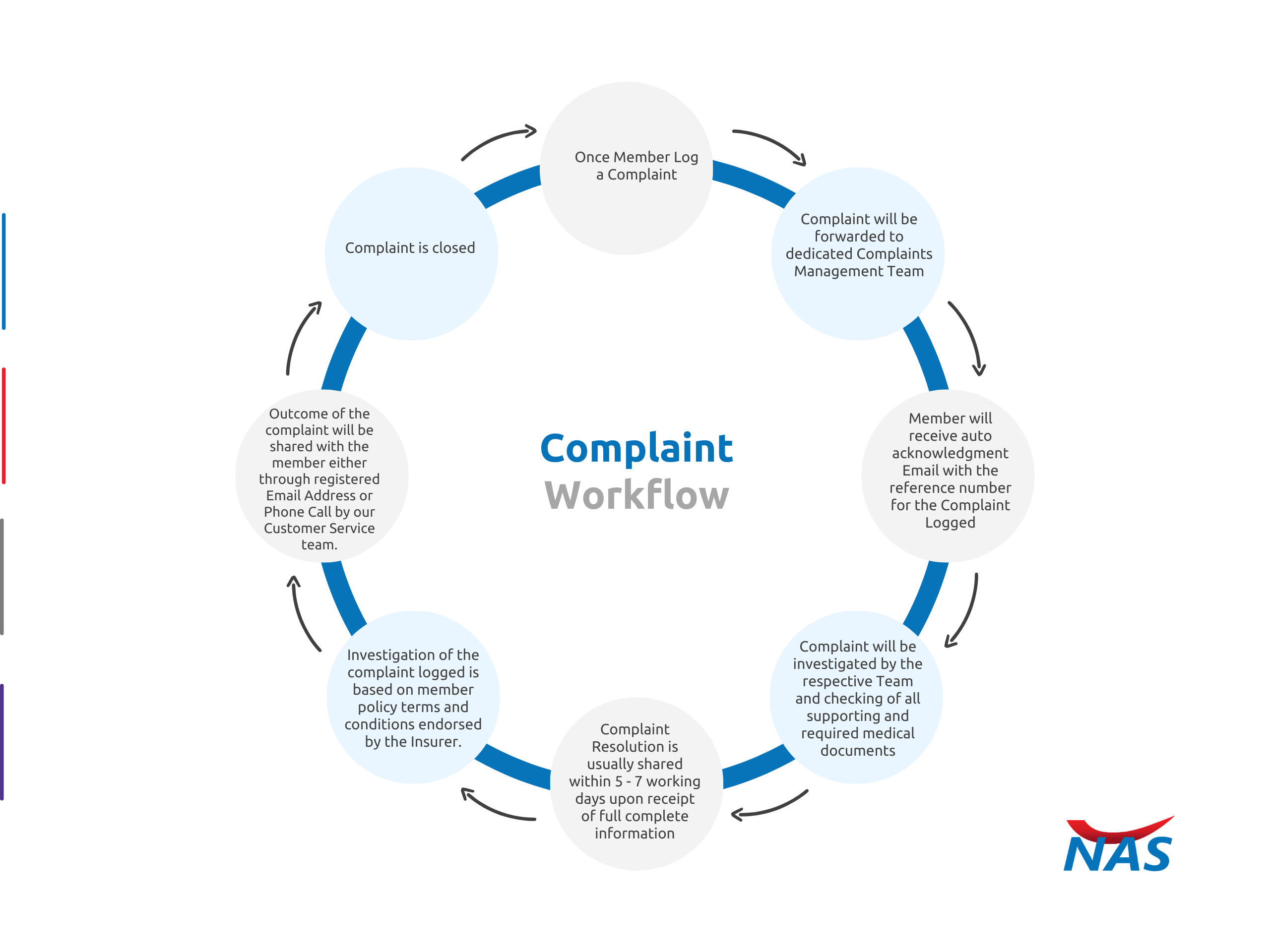
The following shall take place :